What They Don’t Teach You About Refractive Surgery During Training
Erica Liu, MD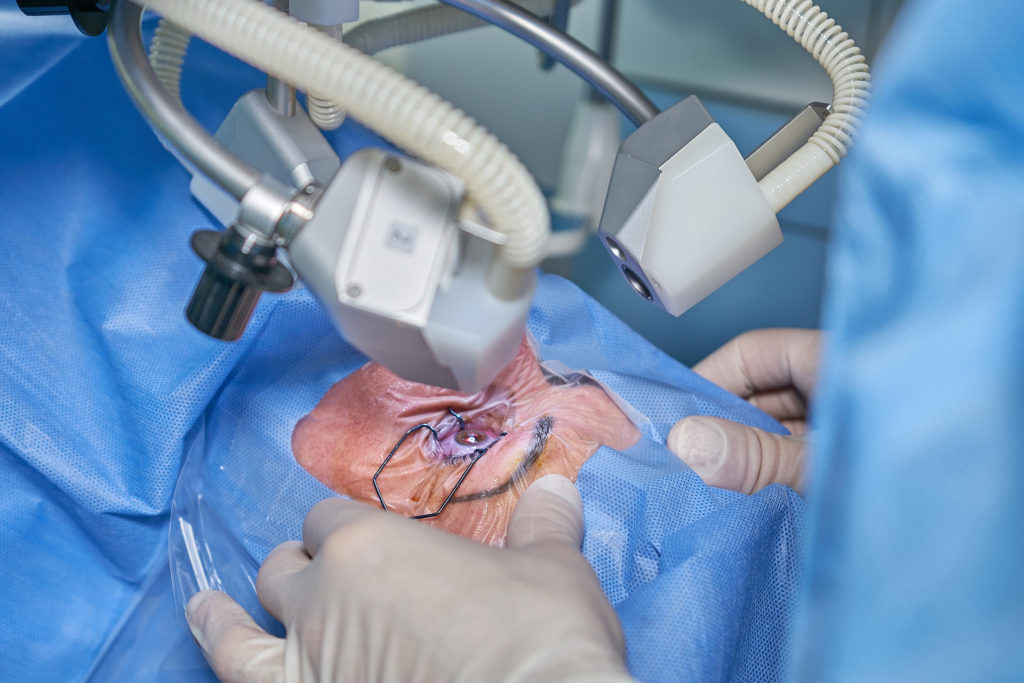
Refractive Training in the US
If you’ve had the average ophthalmology training in the US, you’ve probably had about the same exposure to refractive surgery as you had to contact lens fitting (read: not much). Minimal attention is paid to refractive errors during our training. This domain is mainly left to optometry and is merely an afterthought in ophthalmology. Despite having the ability to surgically fix refractive errors safely and predictably, refractive surgery is generally considered a luxury rather than a necessity. It is considered normal to be completely dependent on contact lenses or glasses to function.
According to the World Health Organization, the leading cause of blindness in the world is uncorrected refractive error followed by cataracts. Refractive error, especially myopia, is a growing epidemic throughout the world. The morbidity and economic costs are enormous, estimated to be over $200 billion worldwide annually.
In the US, only a small percentage of ophthalmologists perform refractive surgery. It is unclear why this is the case, though I suspect both lack of exposure and a high barrier to entry both play a role. During training, the majority of programs that even practice refractive surgery keep these self-paying “cosmetic” patients from their trainees. When I was applying to Cornea fellowships, only a handful of programs offered exposure to refractive surgery, and those that did considered 10-20 fellow cases adequate. While this may be enough to understand the mechanics, it is not enough to understand the nuances of patient selection and education.
The Risks & Benefits
As the prevalence of myopia increases, a more balanced view of refractive surgery is imperative to provide our patients with the knowledge to make the right decisions. Refractive surgery’s reputation was likely harmed in the early days, and even still today, by overpromising results and commercialization of what, at the end of the day, is still a medical procedure. LASIK was pushed aggressively and cheapened. There were many ‘LASIK mills’ that performed surgery and abandoned their small percentage of unhappy patients. No wonder the majority of ophthalmologists have decided not to perform the procedure and some even speak out against it. This polarized view is a huge disservice to our patients.
LASIK Misconceptions
LASIK, SMILE, and PRK have come a long way from their inception with new surgical and diagnostic technology and an improved approach to patient selection. The safety and predictability is exceedingly high and has repeatedly been shown to be safer than long-term contact lens use.
Many negative misconceptions of refractive surgery have been disproven with thousands of robust studies, yet patients, and even ophthalmologists and optometrists, continue to perpetuate these false or at the least, incomplete narratives.
For example, surgeons who perform refractive surgery are four times more likely than the general population to have it themselves. I underwent refractive surgery 15 years ago and it was a life changer for me as it is for the vast majority of my patients. Additionally, over a lifetime, refractive surgery is often more economical than contact lenses. For patients, the pandemic has made something that many were just considering become a necessity given supply chain issues, closed offices, increased dry eyes with computer use and fogged, useless glasses with mask wear.
For a more comprehensive list of LASIK myths, this is a well-written summary https://crstoday.com/articles/2016-jul/debunked-lasik-myths-and-misconceptions/.
Normalizing Refractive Surgery
I ended up in a refractive role after fellowship, just by luck, despite my less than ideal view of refractive surgery coming out of training. I hesitated to take the job – it seemed like a copout and waste of my years of training. Now, going on my fourth year however, I’ve learned the impact refractive errors have on our patients are both complicated and consequential. In addition to doing what’s right for our patients, performing refractive surgery is super fun.
There is no other procedure that takes so little time and effort that provides such a rapid improvement in quality of life. A newly established World College of Refractive Surgery and Visual Sciences is committed to increasing education and forging a path to normalizing and standardizing refractive surgery for patients and surgeons.
For the majority of our spectacled pre-cataract patients, laser refractive surgery is their best treatment option. An organ that doesn’t work without a prosthetic device should not be considered our default when we have the technology to fix it. As myopia increases, the need for refractive surgeons and ophthalmologists familiar with refractive surgery will only increase. If our training programs are behind, then it’s on us to inform ourselves and each other so we can help our patients truly understand all their options without false bias.
Donnenfeld E. Debunked: LASIK myths and misconceptions. Cat & Ref Surg Today, 2016: 59-63.
Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, Sankaridurg P. Potential Lost Productivity Resulting from the Global Burden of Myopia: Systematic Review, Meta-analysis, and Modeling. Ophthalmology. 2019 Mar;126(3):338-346.
Kezirian GM, Parkhurst GD, Brinton JP, Norden RA. Prevalence of laser vision correction in ophthalmologists who perform refractive surgery. J Cataract Refract Surg. 2015 Sep;41(9):1826-32.
Masters J, Kocak M, Waite A. Risk for microbial keratitis: Comparative metaanalysis of contact lens wearers and post-laser in situ keratomileusis patients. J Cataract Refract Surg. 2017 Jan;43(1):67-73.
Foo LL, Lanca C, Wong CW, Ting D, Lamoureux E, Saw SM, Ang M. Cost of Myopia Correction: A Systematic Review. Front Med (Lausanne). 2021 Dec 3;8:718724.
